What to Know About Acid Reflux and Burping
Acid reflux happens when contents from your stomach move back up into your esophagus. This action is also called acid regurgitation or gastroesophageal reflux.
If you have symptoms of acid reflux more than twice a week, you might have a condition known as gastroesophageal reflux disease (GERD).
According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), GERD affects about 20 percent of people in the United States. If left untreated, it can sometimes cause serious complications.

GERD symptoms
The main symptom of GERD is acid reflux. Acid reflux can cause an uncomfortable burning feeling in your chest, which can move up into your neck and throat. This feeling is often known as heartburn.
If you have acid reflux, you might develop a sour or bitter taste at the back of your mouth. It might also cause the regurgitation of food or liquid from your stomach into your mouth.
Some other symptoms of GERD include:
- nausea
- chest pain
- pain when swallowing
- difficulty swallowing
- chronic cough
- a hoarse voice
- bad breath
GERD treatment options
To manage and relieve symptoms of GERD, your doctor might encourage you to make certain lifestyle changes, like:
- maintaining a moderate weight, if applicable
- quitting smoking, if you smoke
- avoiding big, heavy meals in the evening
- waiting a few hours after eating to lie down
- elevating your head during sleep (by raising the head of your bed 6-8 inches)
Medication
Your doctor might also suggest taking over-the-counter (OTC) medications like those listed below. All of these medications can cause side effects, so talk with your doctor about which option is the best for you.
Antacids
Antacids like Tums are typically used for occasional and mild symptoms of acid reflux and GERD. But if you find that you’re taking antacids almost every day, you may need a stronger medication.
H2 receptor blockers
H2 blockers like Pepcid AC work to lower the amount of acid your stomach makes. Many H2 blockers are available OTC, while higher doses of these medicines can also be prescribed.
It’s important to note is that one type of H2 blocker — ranitidine (also known as Zantac) — was recently recalled by the FDA for containing the ingredient N-Nitrosodimethylamine (NDMA), which is a known carcinogen.
Proton pump inhibitors (PPIs)
PPIs like Prilosec also lower the amount of acid your stomach makes. Because they tend to work better than H2 blockers, they’re more helpful when it comes to healing the esophageal lining — which can become damaged when someone is dealing with GERD for a while.
Like H2 blockers, you can buy some PPIs OTC, and your doctor can also prescribe you a higher dose.

The problem with home remedies for GERD
Some individuals might prefer to start with home remedies to treat their heartburn. While certain home remedies may help a little when it comes to occasional bouts of acid reflux, if you’ve been diagnosed with GERD, you’re most likely dealing with a chronic issue.
Chronic health issues can sometimes be eased by lifestyle changes, but also typically need some kind of medical intervention. When it comes to chronic issues, it’s best to resist the desire to self-diagnose and self-medicate. Talk with your doctor before starting any new treatments.
A few home remedies floating around out there that may do more harm than good include:
- Drinking a baking soda and water solution. Because baking soda is alkaline, it has the ability to help neutralize acidity, and is mostly safe to consume in small doses. But baking soda is high in sodium, and it’s also possible to experience side effects if you consume too much.
- Chewing gum. The thought here is that because saliva is slightly alkaline, stimulating it by chewing gum after eating may help neutralize the acidity in your mouth and throat. While a very small study from 2005 did find some merit to this approach, the size of the study makes it difficult to draw any real conclusions.
- Consuming ginger. Ginger is a common home remedy for issues like nausea and a sour stomach, but it’s still unclear if it can actually help with occasional heartburn symptoms. In fact, in many studies, heartburn is a symptom of taking too much ginger.
- Drinking milk. Due to its natural alkalinity, milk is another home remedy that’s often touted as a way to ease heartburn symptoms. Unfortunately, even though it may feel soothing initially, the fat and protein it contains can ultimately make heartburn symptoms worse once the milk is digested. Low fat milk may be easier for some people to tolerate.
Diagnosing GERD
If your doctor suspects you might have GERD, they’ll conduct a physical exam and ask about any symptoms you’ve been experiencing.
Your doctor may then recommend you to a gastroenterologist, or may conduct certain tests themselves, including:
- Ambulatory 24-hour pH probe. A small tube is sent through the nose into the esophagus. A pH sensor at the tip of the tube measures how much acid exposure the esophagus is getting, and sends the data to a portable computer. An individual wears this tube for about 24 hours. This method is generally considered the “gold standard” for diagnosisng GERD.
- Esophogram. After drinking a barium solution, X-ray imaging is used to examine your upper digestive tract.
- Upper endoscopy. A flexible tube with a tiny camera is threaded into your esophagus to examine it and collect a sample of tissue (biopsy) if needed.
- Esophageal manometry. A flexible tube is passed through the nose into your esophagus to measure the strength of your esophageal muscles.
- Esophageal pH monitoring. A monitor is inserted into your esophagus to learn how acid is regulated in your body over a period of a few days.
After arriving at a diagnosis, your doctor will decide what interventions will work best for you, and if surgery is an option.
Surgery for GERD
In most cases, lifestyle changes and medications are enough to prevent and relieve symptoms of GERD. But sometimes, surgery is needed.
For example, your doctor might recommend surgery if lifestyle changes and medications alone haven’t stopped your symptoms. They might also suggest surgery if you’ve developed complications of GERD.
There are multiple types of surgery available to treat GERD, including fundoplication (during which the top of your stomach is sewn around your esophagus), and bariatric surgery (usually recommended when a doctor has concluded that your GERD may be exacerbated by too much excess weight).
GERD vs. heartburn
It’s important to note that there’s a very real distinction between occasional heartburn (which may not need medical intervention), and GERD.
Most people experience heartburn from time to time, and in general, occasional heartburn isn’t a cause for concern.
But if you’ve been experiencing heartburn more than twice a week, and especially if you’ve also been experiencing a chronic cough and chest pain, you might be dealing with GERD.
Find out the differences and links between heartburn, acid reflux, and GERD.
GERD causes
While there’s no single cause of GERD, there is a mechanism in your body that — when not functioning properly — can increase the likelihood of it.
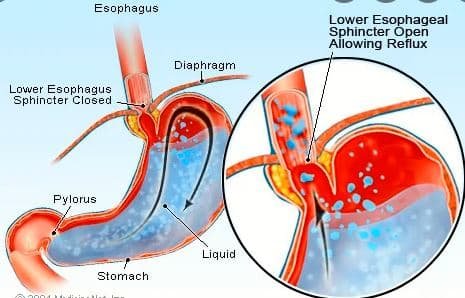
The lower esophageal sphincter (LES) is a circular band of muscle at the end of your esophagus. When it’s working correctly, it relaxes and opens when you swallow. Then it tightens and closes again afterward.
Acid reflux happens when your LES doesn’t tighten or close properly. This allows digestive juices and other contents from your stomach to rise up into your esophagus.
Other possible causes include:
- Hiatal hernia. This is when a part of the stomach moves above the diaphragm towards the chest area. If the diaphragm is compromised, it can increase the likelihood that your LES can’t do its job correctly.
- Frequently eating large meals. This can cause the distension of the upper part of the stomach. This distension sometimes means there isn’t enough pressure on the LES, and it doesn’t close properly.
- Lying down too soon after large meals. This can also create less pressure than the LES needs to function properly.
Risk factors for GERD
While again, there’s no one cause of GERD, there are lifestyle choices and certain health factors that can make a diagnosis more likely. These include:
- living with obesity
- being pregnant
- living with a connective tissue disorder
- smoking
- frequently eating large meals
- consistantly lying down or going to sleep shortly after eating
- eating a lot of certain types of foods, like deep fried or tomato products
- drinking certain types of beverages, like soda, coffee, or alcohol
- using an abundance of nonsteroidal anti-inflammatory drugs (NSAIDS), like aspirin or ibuprofen
Alcohol and GERD
Alcohol consumption and GERD have been connected in many studies, and it seems like the more alcohol you drink, the higher the likelihood you might develop GERD.
While the connection is not crystal clear — does alcohol affect the LES directly, or do people who drink a lot of alcohol also have other behaviors that can lead to GERD? — what is clear is that limiting alcohol intake, or stopping it completely, after you’ve been diagnosed, may provide some symptom relief.
Dietary triggers for GERD
Some people who’ve been diagnosed with GERD find that certain foods and beverages can trigger their symptoms. While triggers can be very personal, there are a few foods that are routinely cited as more triggering than others. They include:
- high fat foods (like fried foods and fast foods)
- citrus fruits and juices
- tomatos and tomato sauces
- onions
- mint
- coffee
- soda
GERD and other conditions
The symptoms of GERD can sometimes be exacerbated by other conditions you may be living with.
Anxiety and GERD
According to research from 2015, anxiety and heartburn can be connected. When one increases in severity, the other might as well. It’s also possible that individuals living with heartburn or GERD are more anxious because living with the condition can produce unwanted symptoms.
If you suspect that anxiety is making your symptoms worse, consider talking to your doctor about strategies to relieve it.
Pregnancy and GERD
Pregnancy can increase your chances of experiencing acid reflux. If you had GERD before getting pregnant, your symptoms might get worse.
Hormonal changes during pregnancy can cause the muscles in your esophagus to relax more frequently. A growing fetus can also place pressure on your stomach. This can increase the risk of stomach acid entering your esophagus.
Many medications that are used to treat acid reflux are safe to take during pregnancy. But in some cases, your doctor might advise you to avoid certain antacids or other treatments.
Asthma and GERD
Asthma and GERD.
While more research is needed to understand the exact relationship between asthma and GERD, it’s possible that GERD might make symptoms of asthma worse. Additionally, asthma and some asthma medications might increase your risk of experiencing GERD.
If you have asthma and GERD, it’s important to manage both conditions.
IBS and GERD
Irritable bowel syndrome (IBS) is a condition that can affect your large intestine. Common symptoms include:
- abdominal pain
- bloating
- constipation
- diarrhea
According to a 2018 review, GERD-related symptoms are more common in people with IBS than in the general population.
If you have symptoms of both IBS and GERD, make an appointment with your doctor. They might recommend changes to your diet, medications, or other treatments.
GERD in infants
It’s normal for babies to spit up food and vomit sometimes. But if your baby is spitting up food or vomiting frequently, they might have GERD.
Other potential signs and symptoms of GERD in infants include:
- refusal to eat
- trouble swallowing
- gagging or choking
- wet burps or hiccups
- irritability during or after feeding
- arching of their back during or after feeding
- weight loss or poor growth
- recurring cough or pneumonia
- difficulty sleeping
If you suspect your baby might have GERD or another health condition, make an appointment with their doctor.
Potential complications of GERD
In most people, GERD doesn’t cause serious complications. But in rare cases, it can lead to serious or even life-threatening health problems.
Potential complications of GERD include:
- esophagitis, an inflammation of your esophagus
- esophageal stricture, which happens when your esophagus narrows or tightens
- Barrett’s esophagus, involving permanent changes to the lining of your esophagus
- esophageal cancer, which affects a small portion of people with Barrett’s esophagus
- tooth enamel erosion, gum disease, or other dental problems
To lower your chances of complications, it’s important to take steps to manage and treat the symptoms of GERD.
Takeaway
If you experience occasional heartburn every so often, you’re not alone.
Treating these occasional occurrences with OTC antiacids and some lifestyle changes, like waiting a few hours to lie down after eating, can usually create relief. But if you find yourself experiencing heartburn more than twice a week and small lifestyle changes don’t seem to be fixing anything, you may be dealing with GERD.
If you’ve been diagnosed with GERD, your doctor will help you come up with a treatment plan that works for you. OTC medication, prescription meds, and even surgery are all options, depending on where you are with the condition.
Don’t let persistent heartburn get in the way of living your life. Talk with your doctor if you believe you may have symptoms of GERD.
How to Prevent Acid Reflux and Heartburn
Acid reflux happens when your stomach acid backs up into your esophagus. Your esophagus is the muscular tube that connects your throat and stomach. The most common symptom of acid reflux is a burning sensation in your chest, known as heartburn. Other symptoms may include a sour or regurgitated food taste in the back of your mouth.
Acid reflux is also known as gastroesophageal reflux (GER). If you experience it more than twice a week, you may have gastroesophageal reflux disease (GERD). In addition to frequent heartburn, symptoms of GERD include difficulty swallowing, coughing or wheezing, and chest pain.
Most people experience acid reflux and heartburn from time to time. GERD is a more serious condition that affects about 20 percent of Americans. Research in the journal Digestive Diseases and Sciences suggests that rates of GERD are rising.
Learn about steps you can take to prevent acid reflux and heartburn. Lifestyle changes, medication, or surgery may help you find relief.

Risk Factors for Acid Reflux and Heartburn
Anyone can experience occasional acid reflux and heartburn. For example, you may experience these symptoms after eating too quickly. You may notice them after consuming lots of spicy food or high-fat treats.
You’re more likely to develop GERD if you:
- are overweight or obese
- are pregnant
- have diabetes
- smoke
Eating disorders, such as anorexia and bulimia nervosa, may also contribute to some cases of GERD. “People who induce vomiting, or have in the past, can have an increased risk of heartburn,” says Jacqueline L. Wolf, M.D., an associate professor of medicine at Harvard Medical School.
Lifestyle Changes
Occasional or mild cases of acid reflux can usually be prevented by adopting a few lifestyle changes. For example:
- Avoid lying down for three hours after a meal.
- Eat smaller meals more frequently throughout the day.
- Wear loose-fitting clothing to avoid pressure on your abdomen.
- Lose excess weight.
- Quit smoking.
- Raise the head of your bed six to eight inches by placing wooden blocks under your bedposts. Bed risers are another option for doing this.
Several types of food can cause acid reflux and heartburn. Pay close attention to how you feel after eating different foods. Your triggers may include:
- fatty or fried foods
- alcohol
- coffee
- carbonated beverages, such as soda
- chocolate
- garlic
- onions
- citrus fruits
- peppermint
- spearmint
- tomato sauce
If you experience acid reflux or heartburn after eating certain foods, take steps to avoid them.

Medication
Many people can resolve their symptoms through lifestyle changes. Other people may require medications to prevent or treat acid reflux and heartburn. Your doctor may recommend over-the-counter or prescription medications, such as:
- antacids, such as calcium carbonate (Tums)
- H2-receptor blockers, such as famotidine (Pepcid AC) or cimetidine (Tagamet HB)
- mucosal protectants, such as sucralfate (Carafate)
- proton pump inhibitors, such as rabeprazole (Aciphex), dexlansoprazole (Dexilant), and esomeprazole (Nexium)
A Note About Proton Pump Inhibitors
Proton pump inhibitors are the most effective treatments for chronic acid reflux. They’re generally considered very safe. They reduce your body’s production of gastric acids. Unlike some other medications, you only need to take them once a day to prevent symptoms.
There are also downsides to using proton pump inhibitors on a long-term basis. Over time, they can deplete vitamin B-12 in your body. Since stomach acid is one of your body’s defenses against infection, proton pump inhibitors can also raise your risk of infection and bone fractures. In particular, they can raise your risk of hip, spine, and wrist fractures. They can also be expensive, often costing more than $100 each month.
Surgery
Surgery is only necessary in rare cases of acid reflux and heartburn. The most common surgery used to treat acid reflux is a procedure known as Nissen fundoplication. In this procedure, a surgeon lifts a portion of your stomach and tightens it around the junction where your stomach and esophagus meet. This helps increase pressure in your lower esophageal sphincter (LES).
This procedure is performed with a laparoscope. You will need to stay in the hospital for one to three days after it’s performed. Complications are rare and the results are extremely effective. However, surgery may lead to increased bloating and flatulence or trouble swallowing.
The Takeaway
If you experience regular acid reflux or heartburn, speak to your doctor. They may recommend lifestyle changes to help prevent your symptoms. For example, they may advise you to eat smaller meals, remain upright after eating, or cut certain foods from your diet. They may also encourage you to lose weight or quit smoking.
If lifestyle changes don’t relieve your symptoms, your doctor may recommend over-the-counter or prescription medications. In rare cases, you may need surgery. Complications from the surgery are rare.

Acid reflux occurs when acid from your stomach flows back up your esophagus toward your mouth. Frequent episodes of acid reflux may be a sign of a condition known as gastroesophageal reflux disease (GERD).
GERD is very common. According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), it affects around 20 percent of people in the United States.
Symptoms of GERD include heartburn, nausea, and a sour taste at the back of your mouth. Burping is also associated with acid reflux and GERD. In particular, people who have GERD often report frequent burping.
Let’s get into how acid reflux and burping are connected, the causes, and what you can do to get relief from burping.
Can acid reflux cause you to burp?
Burping happens when swallowed air escapes from your upper gastrointestinal tract. This is a completely normal occurrence that helps to rid your abdomen of excess air.
According to a 2020 review, it’s normal for a healthy person to burp up to 30 times a day. But acid reflux may cause you to burp more often.
One of the reasons for an increase in burping is because acid reflux increases swallowing. People who experience acid reflux and heartburn tend to ingest air more frequently and in larger quantities, leading to burping.
In addition to acid reflux, your diet and lifestyle, as well as certain medical conditions and medications, can also affect how much you burp.
Diet
Some types of foods are known to trigger burping.
These include carbonated drinks, beer, caffeine, and foods high in fiber, starch, or sugar, such as:
- beans and lentils
- certain vegetables, including peas, onions, mushrooms, cabbage, broccoli, and cauliflower
- some fruits, like bananas
- whole grains
Lifestyle habits
Your day-to-day habits can also trigger burping. Habits associated with excess burping include smoking, sucking on lozenges, and chewing gum.
Talking while eating, eating quickly, and using a straw to drink can all increase burping, too. Wearing dentures that don’t fit properly is another cause of excess belching.
Anxiety and hyperventilating, which can cause you to breathe more rapidly, may also lead to more frequent burping.
Medical conditions
If you burp frequently without experiencing acid reflux or heartburn, another gastrointestinal condition might be the culprit.
Some conditions associated with frequent burping include:
- aerophagia
- celiac disease
- constipation
- gastritis
- gastroparesis
- Helicobacter pylori (H. pylori) infection
- indigestion (dyspepsia)
- irritable bowel syndrome (IBS)
- lactose intolerance
- peptic ulcers
- rumination disorder
These conditions are typically accompanied by other symptoms besides burping.
If you have symptoms other than belching, make an appointment with your doctor to get a proper diagnosis and the right type of treatment.
Medications
Certain common medications, including laxatives and nonsteroidal anti-inflammatory drugs (NSAIDs), may list gas and belching as side effects.
Home remedies for burping
If you find that you tend to burp a lot after eating, the following home remedies may help to ease or reduce your burping:
- Go for a walk after eating. After a meal, light physical activity may help to move food through your digestive tract.
- Take an antacid. If your burping is accompanied by acid reflux or heartburn, an over-the-counter antacid may help.
- Try gas medication. Over-the-counter drugs such as Gas-X and Mylanta Gas contain simethicone, which helps gas bubbles in your stomach bind together. As a result, you may not burp as frequently.
- Chew fennel seeds. In certain cultures, people chew fennel seeds after eating to improve their digestion. While not scientifically proven, fennel seeds don’t carry a serious risk of side effects.
- Drink tea. Some herbal teas, such as chamomile and ginger tea, may improve burping associated with indigestion and acid reflux.
How to prevent burping
The key to reducing how often you burp is to limit how much air you swallow, especially when you eat and drink.
The following tips may help reduce the frequency of your burping:
- Slow down while you’re eating and drinking.
- Avoid talking while you’re chewing your food.
- Try not to gulp drinks and avoid using straws.
- Eat smaller meals.
- Try to cut back on chewing gum and lozenges.
Besides paying attention to your eating and drinking habits, the following may also help reduce how often you burp:
- Try to cut back on foods and drinks known to cause acid reflux and burping.
- Quit smoking. When you inhale cigarette smoke, you’re also swallowing air.
- Try to focus on breathing more slowly. Therapies such as diaphragmatic breathing, alternate nostril breathing, box breathing, and meditation may help.
Reducing stomach acid has been found to reduce burping. A 2012 study found that famotidine, a medication that targets acid reflux, also decreased the frequency of belching.
When to get care
On its own, burping isn’t usually cause for concern. However, if it starts to interfere with your day-to-day life, you might consider talking to your doctor about it.
You should definitely talk to your doctor if frequent burping is accompanied by other symptoms, such as heartburn, abdominal pain, or nausea. These may signal an underlying gastrointestinal problem.
For burping caused by acid reflux, your doctor will likely suggest a combination of medication, diet, and lifestyle changes to target excess acid. Common medications for acid reflux include antacids, H2 blockers, and proton pump inhibitors (PPIs).
The bottom line
Acid reflux can make you burp more often. The reason for this is because having acid reflux increases swallowing. This, in turn, can cause you to ingest air more frequently and in larger quantities.
Treating acid reflux with an over-the-counter antacid may help to reduce burping. You may also be able to reduce the frequency of your burping with lifestyle and dietary changes.
If over-the-counter antacids don’t help, or if your burping is accompanied by other symptoms, it’s a good idea to follow up with your doctor to find out if your burping is due to some other condition.