How to understand digestive disease
How to understand digestive disease AKA gastrointestinal disease
Understanding Peristalsis
Peristalsis is a series of wave-like muscle contractions that move food through the digestive tract. It starts in the esophagus where strong wave-like motions of the smooth muscle move balls of swallowed food to the stomach. There, the food is churned into a liquid mixture called chyme that moves into the small intestine where peristalsis continues.
Stretching out a piece of intestine will make it easier to see the wave-like motion. The motion mixes and shifts the chyme back and forth. This lets the bloodstream absorb nutrients through the walls of the small intestine.
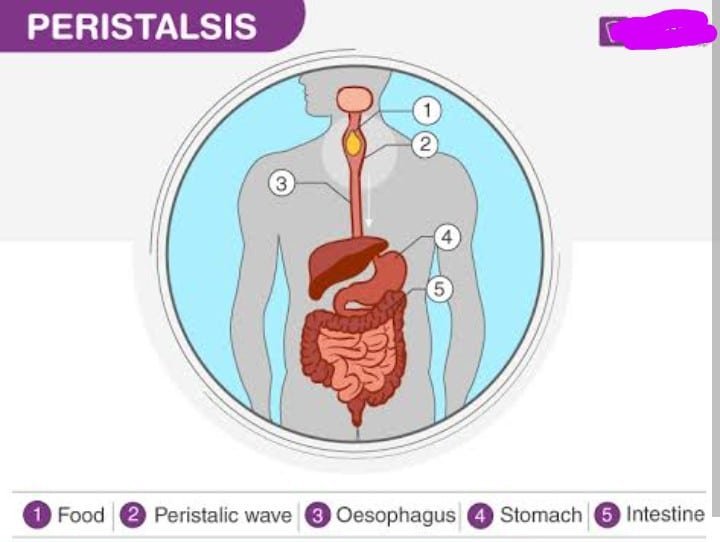
In the large intestine peristalsis helps water from undigested food be absorbed into the blood stream. Then, the remaining waste products are excreted through the rectum and anus.
Digestive Diseases
When you eat, your body breaks food down to a form it can use to build and nourish cells and provide energy. This process is called digestion.
Your digestive system is a series of hollow organs joined in a long, twisting tube. It runs from your mouth to your anus and includes your esophagus, stomach, and small and large intestines. Your liver, gallbladder and pancreas are also involved. They produce juices to help digestion.
There are many types of digestive disorders. The symptoms vary widely depending on the problem. In general, you should see your doctor if you have:
- Blood in your stool
- Changes in bowel habits
- Severe abdominal pain
- Unintentional weight loss
- Heartburn not relieved by antacids
Common digestive problems include the following:
- Constipation
- Diarrhea
- Acid reflux
- Hemorrhoids
Most common digestive problems are short term and easy to control with lifestyle changes and sometimes medication. If symptoms don’t get better, or if they get worse, talk with your health care professional. In some cases, these problems can be a sign of more serious medical conditions.
Constipation
Constipation involves having fewer than three bowel movements a week. Stools may be firm or hard to pass. Your abdomen may feel swollen or bloated.
Common causes of constipation include
- not eating enough fiber
- not drinking enough water
- certain medications
- changes in routine (such as travel)
During pregnancy, increased levels of hormones can slow down the digestive system and cause constipation.
Treatment of Constipation
Constipation may be treated with foods that contain fibres. Fiber is found in plant foods. It’s the part of the plant that your body cannot digest. Fiber passes relatively unchanged through your digestive system. It can help prevent constipation by adding bulk to the stool, making it easier to pass. A fiber-rich diet may also help lower cholesterol levels and help you maintain a healthy weight.
Current guidelines recommend that women eat 25 grams of fiber per day. Most Americans only get about 15 grams per day.
Good sources of fiber include fruits, vegetables, beans, whole grains, and bran. Whole grains include steel-cut oatmeal, brown rice, barley, and corn (including popcorn). Bran is the outer covering of grains such as corn and wheat. It is used as a high-fiber ingredient in cereals and other foods.
Prevention of Constipation
You can help prevent constipation by
- drinking plenty of water
- eating at least 25 grams of fiber a day
- exercising
- not holding your stool (using the bathroom when you feel the urge to have a bowel movement)
Diarrhea
Diarrhea is having three or more loose bowel movements a day. It can also cause cramping.
Causes of Diarrhea
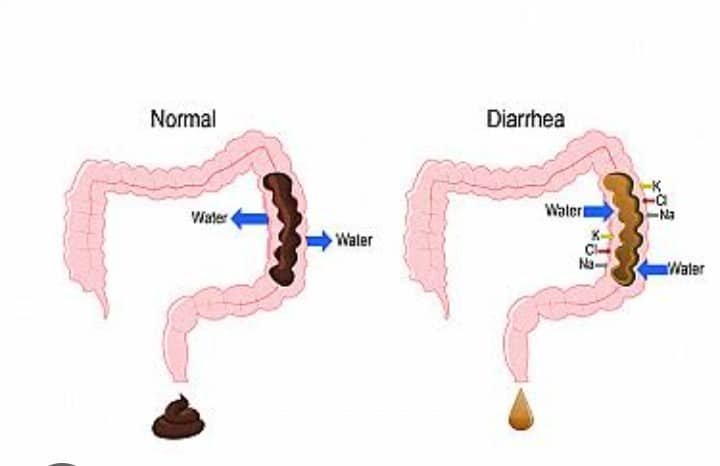
Several things can cause diarrhea:
- Infection with harmful bacteria or viruses, which can be caused by eating or drinking contaminated food or water
- Consuming dairy products (if you are lactose intolerant), caffeine, artificial sweeteners, or certain additives
- Taking medications, especially antibiotics
- Digestive diseases, such as irritable bowel syndrome (IBS)
Symptoms Diarrhea
If diarrhea lasts more than 2 days, see your health care professional. Also see your health care professional if:
- your stools contain blood or pus
- you have a fever
- you have severe abdominal pain
- you have signs of dehydration (thirst, dry skin, fatigue, dizziness, less frequent urination, or dark-colored urine)
You may need tests to find the cause of your diarrhea so that the right treatment can be given.
Treatment of Diarrhea
Diarrhea can cause dehydration (loss of fluids from the body). If you have diarrhea, drink plenty of fluids to replace those that are lost.
If diarrhea does not go away in a few hours, drink fluids and liquid foods that contain salt, such as sports drinks or broth. Avoid drinking dairy products, soda, and juices. They may contain lactose, caffeine, or sugar, which may make diarrhea worse.
Over-the-counter anti-diarrheal medications can be helpful. But they should not be taken if you have a high fever or bloody diarrhea, which can be signs of a bacterial infection.
Acid Reflux
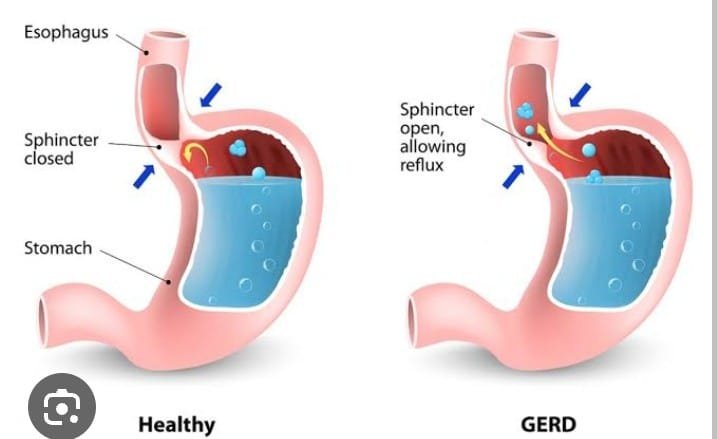
Acid reflux happens when the muscle in your esophagus that opens and closes when you swallow does not work properly. When this happens, food and digestive fluids, which contain acid, back up into your esophagus. Acid reflux can cause a burning feeling in your chest and throat, which is sometimes called heartburn.
Acid reflux is common and usually is not serious.
Certain conditions and habits may trigger acid reflux. You may notice acid reflux more often when you drink alcohol or caffeine or eat certain foods, such as citrus fruits, tomatoes, or fried foods. It may become more frequent while lying down. It happens more often during pregnancy as well as in people who are obese or who smoke.
Control or Prevention of Acid Reflux
Try taking these steps may help to control or prevent acid reflux:
- Raise the head of your bed.
- Eat small, more frequent meals.
- Quit smoking.
- Avoid foods and drinks that make your symptoms worse.
- Avoid lying on your back right after eating.
- Garnish your meals with mixed fruits and vegetables.
- Avoid late evening meals.
Treatment of Acid Reflux
Several over-the-counter medications are available that may help reduce your symptoms. Antacids reduce the acid content in the stomach. Other medications stop the digestive system from making too much acid. Some of these medications are available over the counter.
Gastroesophageal Reflux Disease (GERD)
If acid reflux happens more than twice a week, or if you have been taking over-the-counter medications for more than 2 weeks with no relief, you may have a condition called gastroesophageal reflux disease (GERD). Treatment includes lifestyle changes and medication.
GERD that is not treated can lead to complications, including ulcers in the esophagus, narrowing of the esophagus, and a precancerous condition called Barrett’s esophagus. If you have GERD, it is important to see your health care professional regularly for treatment and follow-up.
Hemorrhoids
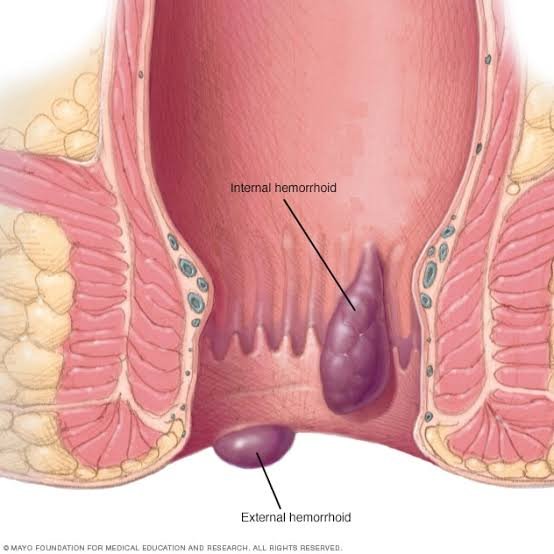
Hemorrhoids are swollen blood vessels in and around the anus and lower rectum. The vessels stretch under pressure. They can become painful, itchy, and irritated. Passing stool may injure the hemorrhoids and cause them to bleed.
Causes of Hemorrhoids
Hemorrhoids can result from several factors:
- Being overweight
- Pregnancy
- Standing or sitting for long periods
- Straining during physical labor
- Constipation (straining to have bowel movements)
Adding fiber and fluids to your diet can help prevent hemorrhoids.
Treatment of Hemorrhoids
The symptoms of hemorrhoids can be relieved with ice packs to reduce swelling. Sitting in a bath of warm water may relieve symptoms. You may also use a hemorrhoid cream or suppositories. If problems do not go away, contact your health care professional. Surgery may be needed to remove hemorrhoids in some cases.
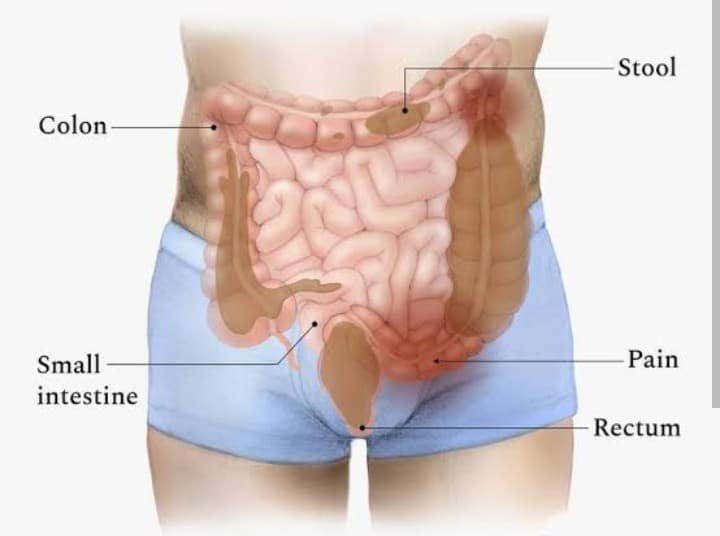
Irritable Bowel Syndrome
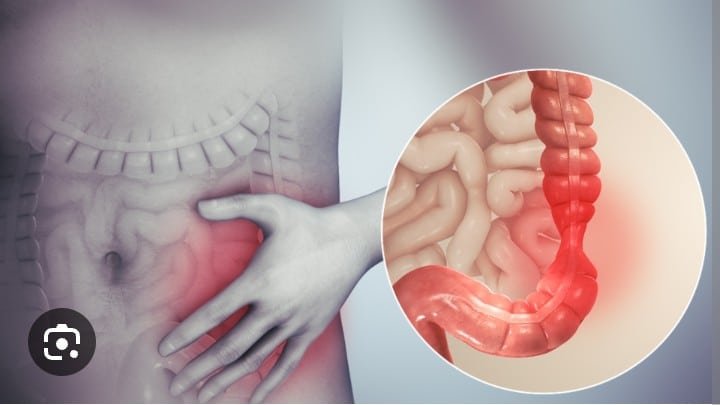
IBS mainly affects women between the ages of 30 and 50. For some people, it is only mildly annoying. For others, it can be serious. Symptoms may include the following:
- Cramps
- Gas
- Bloating
- Changes in bowel habits—constipation, diarrhea, or both
- An urge to have a bowel movement that does not happen
- Stools that have mucus in them.
Causes of Irritable Bowel Syndrome
It is not clear what causes IBS. But stress, eating large meals, or travel may trigger the symptoms. Certain medications or foods can also cause symptoms to flare up. Caffeine, dairy products, and large amounts of alcohol can cause problems as well. Women may have more symptoms during their menstrual periods.
Treatment of IBS
IBS cannot be cured, but it can be managed to reduce the symptoms. You may have tests to help rule out other conditions first.
Your health care professional or a nutritionist can suggest changes in your diet to help manage IBS. Eating frequent small meals rather than two or three large meals a day can help. In some cases, adding fiber to your diet may help. Your health care professional may also suggest medications to relieve the symptoms.
Inflammatory Bowel Disease
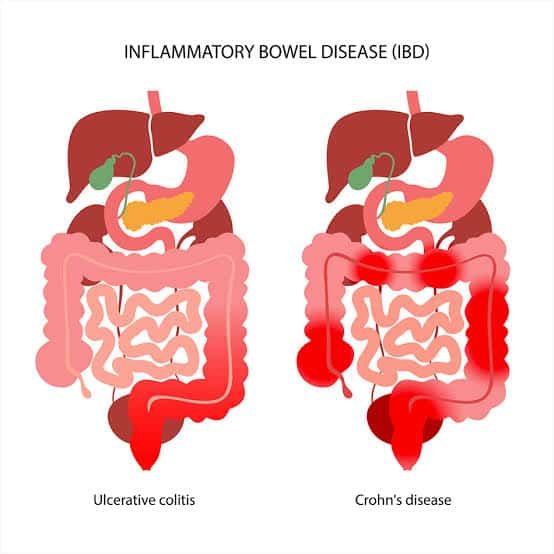
IBD is a group of diseases that cause inflammation throughout the digestive system. If inflammation does not go away, parts of the digestive system can be damaged. There are two main types of IBD:
- Crohn’s disease can affect any part of the digestive system
- Ulcerative colitis usually affects the large intestine (also called the colon)
Symptoms of IBD may include the following:
- Abdominal pain
- Diarrhea that doesn’t go away
- Fatigue
- Stools that have blood in them
- Weight loss
Causes of IBD
It’s not clear what causes IBD, but it may be related to a problem with the immune system. Your genes may be a factor too. Your health care professional may do several tests to make sure that your symptoms are caused by IBD and not caused by an infection.
Treatment of IBD
IBD is usually treated with medication first. But if the damage is severe, surgery may be an option.
Celiac Disease
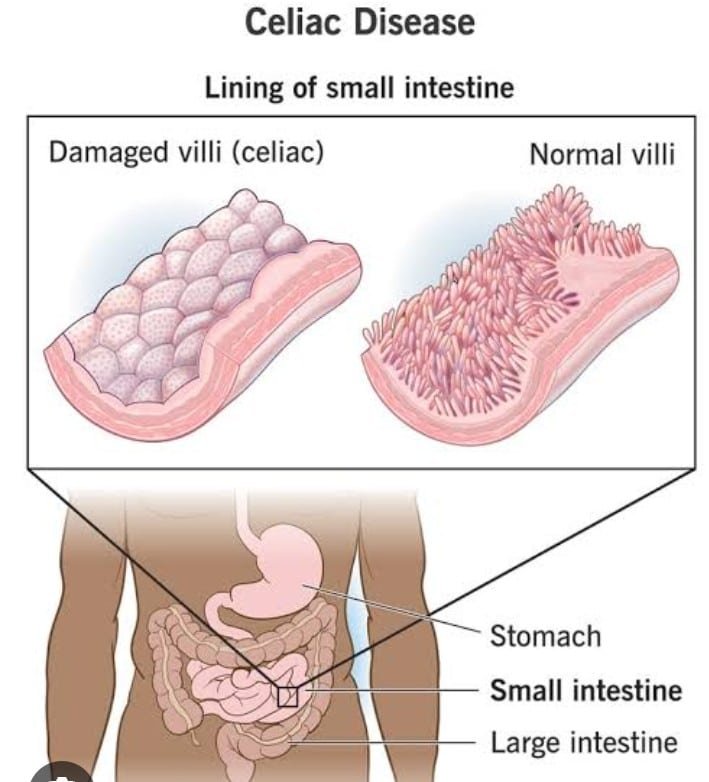
People with celiac disease cannot tolerate gluten, a protein found naturally in wheat, rye, and barley. Gluten is also added to certain food products.
When gluten is eaten, the immune system reacts by damaging the lining of the small intestine. Because of this damage, nutrients cannot be absorbed properly.
Celiac disease is one of the most common digestive disorders, affecting about 1 in 133 people.
Symptoms of Celiac Disease
Some people with celiac disease have no symptoms. Others may have
- diarrhea
- constipation
- fatigue
- abdominal pain and bloating
Diagnosis od Celiac Disease
If your health care professional thinks that you may have celiac disease, the first step is to have a blood test. This test looks for certain antibodies that show that the immune system is reacting against gluten. If the antibodies are found in your blood, you may have a biopsy of the intestine to look for damage and confirm the diagnosis.
Treatment of Celiac Disease
If celiac disease is not treated, the disease can increase the risk of serious health problems, including osteoporosis, anemia, and cancer. Treatment involves avoiding gluten in your diet. Researchers are also studying medications that can make gluten less toxic to the small intestine.
Colorectal cancer
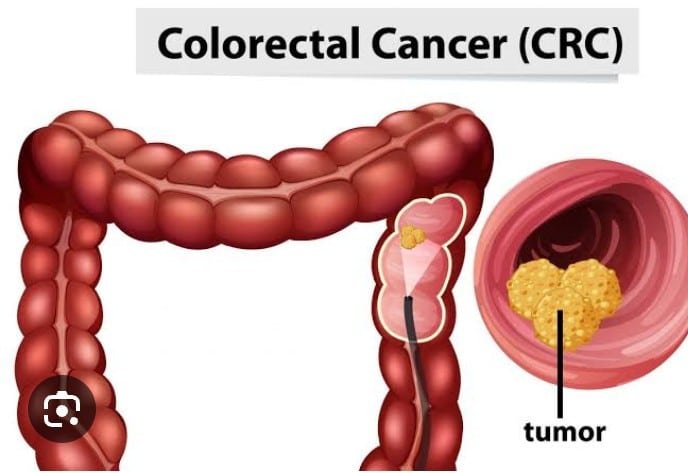
Colorectal cancer is cancer of the rectum and colon. It is the second leading cause of cancer death among women in the United States. In most cases, colorectal cancer develops slowly over time. It often begins as a polyp—a tissue growth in the colon or rectum.
Routine screening can help prevent colon cancer. Polyps that are found during routine screening can be removed easily before they become cancerous.
Symptoms of Colorectal Cancer
Colorectal cancer usually shows no signs in the early stages of the disease. In the more advanced stages, signs and symptoms may include the following:
- A change in bowel habits
- Bleeding from the rectum
- Blood in the stool
- Stools that are more narrow than usual
- Abdominal discomfort (bloating, cramps, or frequent gas pains)
- A feeling that you need to have a bowel movement (that does not go away after a bowel movement)
- Loss of appetite
- Weakness and feeling tired
Having these symptoms does not mean that you have cancer. The same symptoms can be caused by other digestive disorders. Talk with your health care professional if you have any of these symptoms.
Risk Factors of Colorectal Cancer
You are at high risk of colon cancer if you
- have a first-degree relative (a parent or sibling) younger than 60 with colorectal cancer or colon polyps
- have two or more first-degree relatives of any age with colorectal cancer or colon polyps
- have had colorectal cancer
- have had colon polyps
- have a family history of familial adenomatous polyposis or hereditary nonpolyposis colon cancer
Lifestyle can play a role in your risk of colorectal cancer. The following factors can increase your risk:
- Eating a diet that is low in fiber and high in fat
- Not exercising regularly
- Being overweight
- Smoking cigarettes or drinking large amounts of alcohol
Treatment of Colorectal Cancer
If your health care professional determines that you have colorectal cancer, there are several treatments available, including surgery, radiation therapy, chemotherapy, and more. Learn about cancer treatment by visiting the websites in the Resources section below.
Credit: medlineplus.gov, acog.org




